I strongly support the motion moved by Ms He Tingru and Mr Leon Perera that this House affirms that gender equality requires a whole-of-society effort to remove all barriers in order to empower every woman to freely realise her full potential and participation in society.
I would like to focus on three areas that I believe will bring us closer towards achieving gender equality in Singapore: residency and benefits for foreign spouses, support for single parents and flexible work arrangements.
Residency and benefits for foreign spouses
According to an answer to a PQ I asked last September, in the six months from February to July 2020, the Immigration and Checkpoints Authority (ICA) received 8,395 applications for extensions of Short-Term Visit Passes (STVP) from foreign spouses of Singaporeans. This was an increase of almost 2,000 applications from the year before. These extensions are typically for one to three months, but some are reportedly as short as one or two weeks. While the vast majority of applications are approved, over 250 were rejected during this six month period last year.
A number of my constituents have sought assistance regarding renewals of STVPs and applications for Long Term Visit Passes (LTVP) for their foreign spouses. I am sure many MPs would have also submitted such appeals to ICA.
In the majority of cases that I have come across, the foreign spouse is a woman. They face the uncertainty and anxiety of being separated from their Singaporean husbands — and in some cases, their children as well — if their passes are not renewed.
I have also noticed that almost all of the residents who have approached me for assistance with their spouses’ visas are from lower income households. Applications for STVP extensions cost $40 for every three months of stay. While it may not seem much, this cost adds up over time. More importantly, their spouses’ immigration worries often add to their daily stresses of life.
To reduce the immigration-related stressors faced by Singapore citizens and their foreign spouses, I propose the creation of a more streamlined path towards obtaining LTVP, LTVP+ and PR status, and eventually citizenship for such spouses.
There are strong reasons to pursue such a policy. For example, given that a quarter of marriages here are between a Singaporean and a non-resident, transnational marriages will continue to be an important contributor to family formation in Singapore. As such, fast-tracking parents, and potential parents, of Singaporean children for citizenship would facilitate the formation of stable family units with a full stake in Singapore.
Towards this end, the primary consideration for a PR application by LTVP holders who have a Singaporean spouse or child, should be their family ties and rootedness in Singapore — and not just their income or occupation. Their close family relationship with Singaporeans makes them part of the Singapore Core and we should facilitate, not inhibit, their integration into our society.
I am aware that not all foreign spouses may immediately qualify for PR status. However, foreigners who have entered into a bona fide marriage with a citizen should be granted LTVP status by default. I have constituents who have been married to foreigners for over a year and are still unable to obtain an LTVP for them. They need to continually renew their spouse’s STVPs, with no certainty of approval each time.
One constituent told me of his desire to have children with his wife but he has shelved those plans because he is worried that his wife may be forced to leave Singapore if her pass is not extended, leading to a separation from any children they might have. Madam, our citizens and their foreign spouses deserve a better assurance of their place in Singapore.
Support for single parents
Next, I would like to appeal for the Government to raise the level of support currently given to single parents, so that they and their children are not disadvantaged in our society. In a speech in 2013, I outlined the burdens faced by single parents who have to take on the role of both father and mother and perform caregiving duties while also holding onto a job to pay the bills. Compounding their challenges, they are denied some of the parenthood benefits that married, divorced and widowed parents receive. This could add to their feeling of marginalisation from society.
Since single mothers make up the bulk of single parents, changes in policies to support single parents will disproportionately benefit women. My former parliamentary colleagues, in particular Ms Lee Li Lian, as well as Dr Daniel Goh, Mr Png Eng Huat; and current MPs Mr Faisal Manap, Mr Dennis Tan, Mr Leon Perera and others have repeatedly advocated for greater support for single parents over the past eight years.
Government benefits and housing options for single unmarried parents and their children should be the same as for any other family unit. The distinction that the Government often makes between single unmarried parents and divorced parents, in terms of the benefits provided, should be removed.
To be clear, we should not encourage single parenthood or having children outside of marriage, any more than we encourage divorce. It is hard enough raising children with both parents, let alone by oneself. However, once a woman has made the brave choice to carry her child to term despite not having the support of a spouse and likely family disapproval, we as a society must do all we can to support her. We should not make things more difficult for her by denying her benefits available to other parents.
We must also be mindful that unequal benefits inadvertently penalise the innocent children of single unmarried parents, who are often in need of greater support. According to a reply to a PQ by Mr Louis Ng, the median monthly income from work of single, unmarried mothers below the age of 35 was just $600 in 2017, which was 86% less than the national median income that year. Currently, many young single parents are not eligible to buy or rent a subsidised HDB flat to live with their children.
What this means in practice — and I have seen this among my constituents — is that they and their children have to squeeze into a flat with their parents, close relatives or friends. However, this is an inherently unstable arrangement. If they fall out with a family member, or are estranged from their families – as some are – they risk having nowhere to stay. Renting a flat in the open market is seldom a realistic option as it is prohibitively expensive. Singles below the age of 35 do not qualify to purchase HDB flats or rent flats under the Public Rental Scheme.
I note that HDB has said it will exercise flexibility in allowing unmarried parents to buy a 3-room or smaller flat in a non-mature estate from HDB, or a resale flat, and those who cannot afford to buy a flat may be considered for public rental flats. I would like to see this made the default for all single parents so that they are not denied a roof over their heads, and their children have a safe and homely environment to grow up in.
Single parents awaiting the construction of their BTO flats should also be allowed to rent a flat under the Parenthood Provisional Housing Scheme (PPHS), which is currently available only to married couples, divorcees or the widowed.
All single parents and their children are a family in every sense of the word, and should be considered a family nucleus by HDB for the purpose of purchasing or renting flats.
Some single parents who are divorcees also continue to face difficulties getting their monthly maintenance from former spouses. The Government introduced the Maintenance Record Office (MRO) scheme in 2016 to assist the courts by identifying those who refuse to pay even though they have the means to do so, so that the courts can impose penalties on them. Mr Leon Perera previously asked in 2017 if MSF could provide a mechanism for spouses to request for an investigation of the MRO without having to go through a Court process. I hope the Ministry will give consideration to this proposal as it reviews the MRO programme.
I should also mention that we should give single fathers the same benefits as single mothers, as they face very similar challenges as single mothers in raising children alone. The Women’s Charter was changed in 2016 to allow men to apply for alimony. However, this is only possible if he is incapacitated and therefore is unable to work. This high bar should be removed. A man should be allowed to apply for maintenance from his ex-wife if he has custody of their children and has a much lower earning power than her.
Flexible work arrangements
The final point I wish to raise relates to work arrangements.
I call for companies to redouble their efforts to make flexible work arrangements available to employees who can and wish to work from home. The Government can do its part to nudge enterprises in this direction through tax incentives and by leading the way through civil service human resource policies.
I recently met an elderly constituent at the wake of her deceased husband. As was my usual practice, I asked if she was in need of any assistance. I was glad to hear that she was doing fine as she was able to continue working from home because of the arrangements made by her enlightened employer. Her employer couriers her work to her flat daily and picks it up from her the next morning after she has completed it. This way, despite her inability to walk very far unassisted, she can apply her skills and earn some income to support herself.
I believe that more businesses should explore such flexible work arrangements to meet their manpower needs while providing employment to those who can only work from home.
This will empower many women with caregiving responsibilities, not to mention older workers and those with mobility issues. There are many women as well as some men who make a difficult choice to stop work temporarily to care for their young children or elderly parents. Very often, this dilemma could have been avoided if more companies allowed their employees to work from home.
One silver lining of the Covid-19 pandemic is that it has forced many companies to digitalise and make work from home arrangements. This has been helpful to many caregivers who need to look after their young children or elderly parents.
However, once Singapore starts to reopen, many companies may start summoning their workers back to the office. I hope companies will not forgo their digital gains this way. Companies should assess which jobs can be performed as productively at home as in the office, and give employees a choice of working remotely.
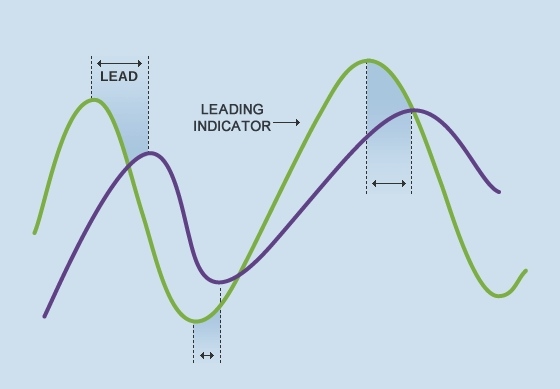
The labour force participation rate of women trails 14% behind men. The gap starts to form for women starting from their mid-twenties — the age when they start having children — and continues to increase throughout their childbearing years, with a peak of some 25% behind men of the same age.
This could point to what is known as a “child penalty”, which can have a negative impact on a woman’s earning power and retirement adequacy. Even with work from home arrangements, SMU sociologist Aliya Rao found that women bear a greater burden of handling both paid work as well as the unpaid work of managing the household. This is a point that Ms He Tingru also made earlier.
The key point here is flexibility. We need to promote a work environment that is more understanding of the various roles mothers and fathers desire to play, and avoid forcing them to choose one role over another. This will enable many more parents to continue pursuing their careers while providing for themselves and caring for their families.
Summary
In summary, I call for the streamlining of immigration procedures for foreign spouses of Singapore citizens to strengthen the Singapore Core; for more support to be extended to single unmarried parents; and for policies to promote flexible work arrangements, all of which will benefit both women and men.
I made this speech in Parliament on 3 August 2021 on a private member’s motion moved by Workers’ Party MPs He Tingru and Leon Perera on Empowering Women.